Facts about Medicaid

Medicaid has grown since its founding in 1965 to become a central part of the American health care system.

Medicaid is an entitlement program that provides medical coverage to those individuals who meet certain eligibility criteria.

Early and Periodic Screening, Diagnostic and Treatment (EPSDT) is a mandatory Medicaid program for children that focuses on prevention and early diagnosis and treatment of medical conditions.

Another area of social concern in regards to Medicaid eligibility is that of the underinsured, or people with declining employee sponsored insurance (ESI) whose private coverage, however ineffective, may disqualify them from Medicaid.

Medicaid planners typically advise retirees and other individuals facing high nursing home costs to adopt strategies that will protect their financial assets in the event of nursing home admission.

The problem is that there are still many in such a situation who are not eligible for Medicaid.

Medicaid is the United States health care program for individuals and families with low incomes and resources.

The Omnibus Reconciliation Act of 1993 (OBRA '93) amended Section 1927 of the Act as it brought changes to the Medicaid Drug Rebate Program.

Medicaid covered five million adults aged over 65; it is the largest single purchaser of nursing home and long-term adult care in the United States in 2001.

At the beginning of the twenty-first century, Medicaid funding became a major budgetary issue for many states, with on average, 16.8 percent of state general funds being spent on the program.

The blind and disabled comprised approximately 17 percent of Medicaid recipients in 2001.
Medicaid covered 24 million low-income children, and 9.3 million low-income adults in families with children in 2001.

States administer their own Medicaid programs, while the federal Centers for Medicare and Medicaid Services (CMS) monitors the state-run programs and establishes requirements for service delivery, quality, funding, and eligibility standards.

Medicaid provides the largest portion of federal money spent for health care on people living with HIV/AIDS.

More than half of people living with AIDS are estimated to receive Medicaid payments.

State Medicaid programs do not consider the value of one's home in calculating eligibility, therefore it is often recommended that retirees pursue home ownership.

Some middle to high-income individuals may qualify for Medicaid benefits over their lower-income counterparts because their ages, illnesses, or disabilities do happen to fit said guidelines.

The solution to this, however, lies not just in reforming Medicaid but in the wider issues of health insurance and entitlement programs in general.

Child welfare agencies ensure that foster children, as well as those in adoption placement, are eligible for Medicaid benefits.

Medicaid is a means-tested program that is not solely funded at the federal level.

Some individuals are eligible for both Medicaid and Medicare (also known as Medicare dual eligibles).

All but a few states use managed care to provide coverage to a significant proportion of Medicaid enrollees, with approximately 60 percent of enrollees in managed care plans.

Medicaid also benefits most wards of the state, such as children in group homes, children pending adoption, and foster children.

By adopting such strategies, many seniors hope they will quickly qualify for Medicaid benefits if the need for long-term care arises.

Medicaid was first enacted on July 30, 1965, through Title XIX of the Social Security Act.

A child may be eligible for Medicaid regardless of the eligibility status of his or her parents or guardians.

Medicaid does not pay benefits to individuals directly; it sends benefit payments to health care providers.

Nor does a middle class or higher income necessarily disqualify from Medicaid benefits.

Medicaid is very different from Medicare, a social insurance program aimed to benefit the elderly and individuals with certain disabilities, with which it is often associated.

In an attempt to limit this practice, some states have a “spend down” policy in which higher-income individuals must spend down or decrease their real assets in order to qualify for Medicaid benefits.

Core eligibility groups of poor children and parents are most likely to be enrolled in managed care, while the aged and disabled eligibility groups more often remain in traditional "fee for service" Medicaid.

Each state operates its own Medicaid system, but this system must conform to federal guidelines in order for the state to receive matching funds and grants.

Unfortunately, Medicaid does not benefit all individuals in need of it, due to strict qualifications regarding age/disability category, income, and assets.

Significantly, Medicaid has reshaped the provision of medical care for many of those who previously saw health care providers less often, if at all, due to lack of health insurance and personal funds.

The DRA also requires that anyone seeking Medicaid must produce documents to prove that he or she is a United States citizen or resident alien.

Being poor, or even very poor, does not necessarily qualify an individual for Medicaid.

Medicaid finances health needs throughout the life cycle: From births to nursing home care.

The main criterion for Medicaid eligibility is limited income and financial resources, a criterion which plays no role in determining Medicare coverage.

Under managed care, Medicaid recipients are enrolled in a private health plan, which receives a fixed monthly premium from the state.
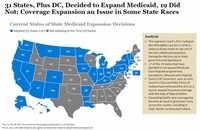
State participation in Medicaid is voluntary; however, all states have participated since 1982, when the last state to join, Arizona, formed the Arizona Health Care Cost Containment System (AHCCCS) program.

Before Medicaid, many individuals saw health care providers only rarely, if at all, and were unable to cover medical costs, whereas those with greater resources or health insurance were able to receive medical attention.

Among the groups of people served by Medicaid are eligible low-income parents, children, seniors, and people with disabilities.

Medicaid was created on July 30, 1965, through Title XIX of the Social Security Act to help individuals who have no medical insurance or poor health insurance.

The Medicaid Drug Rebate Program was created by the Omnibus Reconciliation Act of 1990.

During the 1990s, many states received waivers from the federal government to create Medicaid managed care programs.

Despite its limitations, Medicaid has significantly improved the health care opportunities for many.

In 2001, about 6.5 million Americans were enrolled in both Medicare and Medicaid.


